|
■
Home ■ site map |
||||||||||||||||||||||||||||||||||||||||
|
|
BLOG: June 2010 - December 2013 II - Mammography 10. Mammography risks and harmsEver since the introduction of mammographic X-ray screening as a part of the U.S. public breast cancer policy - and we are talking decades here - public was told that the risks to its users limit to possible discomfort/pain due to breast compression, relatively rare false negatives and not so rare but-nothing-really-there-to-worry-about false positives. Irradiation from screening was labeled as too low to do any harm, and overdiagnosis and overtreatment - who ever heard of them, anyway? Not that those acknowledged risks were taken too seriously, or even presented accurately. For instance, false negatives of mammography screening are not a "minor negative". They are significant problem, and so are false positives, as illustrated toward page bottom. Similarly, despite about half of the women finding breast compression during mammography session painful, and half of those declining invitation to the second round of screening citing the pain as important reason, it is mentioned in less than half of 31 invitations in English speaking and Scandinavian countries with public-funded screening programs. USPSTF's (U.S. Preventive Services Task Force) take on this subject is pretty cryptic: it first states that "compression may add to the discomfort of mammography for some women" and then, citing a systematic evidence review, it makes it "many women", in the very unspecific 1-77% range (Nelson et al. 2009). The Nordic Cochrane Center is more specific; citing the same reference (Armstrong et al. 2007) as USPSTF, and two others, it states that about half of the screened women experience pain from breast compression. And, according to yet another study, in half of women who decline invitation to a subsequent round of screening, as mentioned, pain from compression is a major reason (Screening for breast cancer with mammography, Gøtzsche and Nielsen, 2009). Not one of 31 invitations even mentioned overdiagnosis and overtreatment, which refer to the "diagnosis" and "treatment" of abnormal growths - or what appears to be such - that would not evolve in breast cancer (BC). It is defined as the excess of diagnosed breast cancers in the screened vs. control population in a longer period of time (decade, or more). According to recent research, the rate of overdiagnosis/overtreatment is anywhere between 20% and 50%, with the most likely overall level being about 30-40%. This means that about one in every four breast cancers diagnosed with screening mammography would have never become real cancer. The only radiation risk mentioned in the leaflets is that from screening alone, generally presented as low enough to be of no concern. What leaflets do not mention is the risk of radiation from unnecessary treatment of "cancers" that would have never become health-threatening. And that research indicate that radiotherapy could double mortality from lung cancer and heart disease. Even radiation delivered by screening alone can bi significant risk for women who are more or much more sensitive to radiation - such as those with predisposing genetic polymorphism - and women have every right to know it. Also, most leaflets go on to add that early detection spares women from more invasive treatment, including mastectomies. The reality of it is less comforting: according to the systematic analysis of all large breast cancer randomized controlled trials by the Nordic Cochrane Center, the rate of mastectomy and lumpectomy was 35% higher in the screened population, rate of radiation treatment 32% higher, and chemotherapy rate 4% lower. Which suggests exactly the opposite: the
X-ray screened women get more of In a word, the risk inventory of screening mammography turned out to be much larger than what women were, and still are being told. At the same time, as we've seen on previous pages, its actual benefits shrunk down from certain and sizeable, as advertised for decades, to border insignificant. Summing it up, X-ray mammography risks stem not only from its imperfect detection rate (i.e. false positives and negatives), but also from its higher sensitivity to detect apparently abnormal growths combined with inaccuracy in diagnosing their true nature, resulting in overdiagnosis and overtreatment. In addition, it poses radiation risk, and not primarily due to the radiation exposure during screening procedure; rather due to exposure due to unnecessary radiation treatment of pseudo-BC. Finally, its effect on all-cause mortality rate cannot be, at present, determined with certainty; therefore, the possibility that it increases total mortality rate cannot be excluded. Its net effect, after offsetting potential risks and benefits, seems to be anywhere from negative to marginally positive, depending on the individual situation.
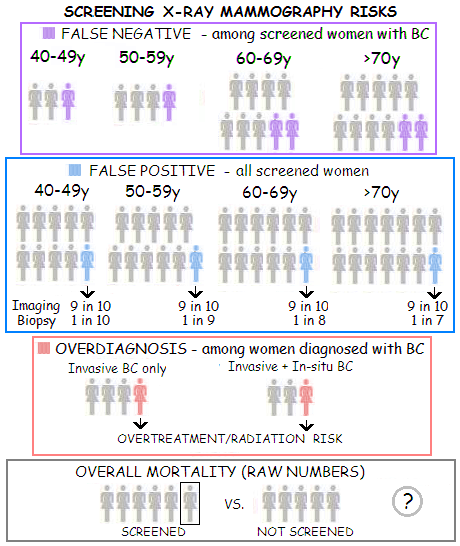
Table bellow shows summary of the risks
associated with screening mammography.
* 1-2 based on Screening for Breast Cancer: Systematic Evidence for the U. S. Preventive Services Task Force, Nelson et al. 2009 (Table 3) Data for the first two screening risks - false negatives and positives, the latter including related additional imaging and biopsies - are based on the latest USPSTF report (2009), thus can be considered conservative (i.e. biased in favor of screening). The hotly debated risk of overtreatment stemming from overdiagnosis would be, according to the USPSTF, contained by the 1-10% overdiagnosis range, which the agency derives from a few biased sources that it chose to use. It neglects the least favorable - and best documented - portion of the evidence, which suggests that the overall rate is much higher, with the worst documented cases exceeding 50%. There is no research on the risk related to breast compression. It may not be significant, but there is no basis to proclaim it negligible. Quite solid evidence suggests that prolonged mild to moderate breast compression (such as that from wearing bra) can be significant breast cancer risk factor, and until there is a reliable research data indicating that screen compression does not pose significant BC risk - at least for some women as well - it should be classified as "unknown" and "potential". The risk of breast irradiation from screening can be at least approximately determined. Although generally low, it can vary significantly with the individual dose of radiation received, and individual vulnerability to the effect of radiation. However, significantly higher risk poses irradiation resulting from unnecessary radiation treatment of overdiagnosed BC (i.e. women with pseudo-disease). It not only increases the risk of getting breast cancer down the road, but probably even more the risk of suffering cardiovascular disease, including the increased risk of dying from it. Finally, the possibility for the screening to result in the higher overall mortality should be taken very seriously. Putting up with "studies were not designed to monitor for this outcome" is no option. As long as this aspect of screening is undetermined, we simply don't know whether X-ray screening of asymptomatic women for breast cancer is beneficial, inconsequential or harmful. The first three risk factors in the above table - false negative, false positive and overdiagnosis - are the consequence of the inaccuracy inherent to the screening mammography test. Illustration below depicts the USPSTF estimates of the rates of false-negative and false-positive from the above table.
As mentioned, the USPSTF's estimates of the false-negative and false-positive rates are not necessarily accurate. Although the database it used (Breast Cancer Surveillance Consortium-BSCS, a collaborative network of five mammography registries and affiliated sites across the United States) includes as many as 600,000 women aged 40 and over, its data structure does not allow for good assessment of all aspect of screening efficacy. For instance, Nelson et al. note that the rates of additional imaging and biopsies for women with false positive tests, as given in their USPSTF report, may be underestimated. The rate of overdiagnosis, which seems to be not accessible from the BCSC data, is shown as 1 in 3, i.e. one out of every three women diagnosed with breast cancer after having a positive mammogram, would not suffer breast cancer symptoms in their lifetime. The range for overdiagnosis rate in well documented sources is 20%-50%, with the simple average of 35% being closest to 1 in 4 rate (overdiagnosis % indicates the % of BC diagnosed over the number of real cancers, which are taken as 100%; so 30% overdiagnosis means that the total of diagnosed BC vs. true BC relates as 130 vs. 100, i.e. 3 pseudo cancers in every 13 diagnosed). This figure is for invasive BC only. For both, invasive and in situ BC, overdiagnosis rate is probably around 50%, or one pseudo-BC in every three diagnosed. Raw numbers from the three adequate random controlled breast cancer trials indicate that for every five all-cause deaths in the unscreened population, there is six all-cause deaths in the screened population (all trials combined give slightly higher all-cause mortality for the screened population: 12 unscreened for every 15 screened). The source data are not sufficiently reliable, though, since no BC trial was designed, or sufficiently powered in the first place, to monitor for this outcome. Following pages address each of the risks of screening mammography in more details. YOUR BODY ┆ HEALTH RECIPE ┆ NUTRITION ┆ TOXINS ┆ SYMPTOMS |
|||||||||||||||||||||||||||||||||||||||