|
■
Home ■ site map |
|||||||||||||||||||
|
|
BLOG: June 2010 - December 2013 I - Breast cancer risk factors 6. Factors predisposing for breast cancer: DietUndoubtedly, diet can play significant role in the development of breast cancer. Food is literally our lifeline, on which we are entirely dependant for support to body functions and regeneration. It has also become a major window of exposure to toxic substances, including carcinogens. Yet, research seems unable to produce solid evidence - or even conclusive evidence of any kind - that this is the case. What is going on? Considering relatively low interest of modern medicine - and even lower level of knowledge of the modern breed of medical professional and researcher (hat off to the exceptions!) - when it comes to food and incredibly complex molecular microcosm in which nutrients and other food ingredients are the very basic factor determining one's wellbeing, this is not much of a surprise. Nor is surprising that there is so much rambling and confusion piling up with every new breast cancer study. If such a major factor as it is the flow of nutrients within the body, body's toxic exposures (with often no clear dividing line between the two), or exposures to radiation are only partly monitored, or not at all, what else can be expected? Not controlling significant factors in any study will randomly distort its findings, and we will end up with the confusing cacophony of studies with
inconclusive, exactly what we have now. That's how we get studies indicating that smoking is protective against breast cancer (Gammon et al., Cigarette smoking and breast cancer risk among young women [United States]). It doesn't help that experimental methods and techniques are often not up to the task of providing reliable information. And even less are subjective, incomplete information sources such as food questionnaires. On top of that, with breast cancer latency period not seldom running into decades, most studies do not span sufficiently long period of time to effectively link breast cancer incidence with its origins. It is probably safe to assume that most of them were analyzing the effect of a limited, insufficient set of factors at a wrong time, after many a cancer had already been initiated and growing. Much less such studies can account for the factors resulting from parental exposures, fetal exposures, or exposures during adolescence, when sensitivity is significantly higher than during adult life - which is the age group focused on by the majority of breast cancer studies. For instance, between 1979 and 1982, levels of PCBs and DDE (DDT metabolite) in blood and breast milk were measured in hundreds of pregnant women in North Carolina (Rogan et al., U.S. Institute for Environmental Health and Sciences), as well as in the fetal blood of their babies. Then 600 babies were followed through their development. Girls with the highest level of fetal exposure to these environmental estrogen mimics, entered puberty nearly a year earlier than those with low exposures. A solid indicator of elevated levels of estrogen, well recognized breast cancer risk factor. And that is only exposure to two chemicals. What does all this have to do with a diet? Well, most of our exposure to environmental estrogens is through food and liquids we consume. And that is just one among many diet-related factors nearly entirely neglected in trials attempting to relate breast cancer incidence to a more or less randomly selected, small number of dietary factors. For instance, a Swedish study (Conjugated linoleic acid intake and breast cancer risk in a prospective cohort of Swedish women, Larsson et al. 2009) investigated possible effect of conjugated linoleic acid (CLA, the linoleic acid form that occurs in dairy products and some meats) on breast cancer incidence by estimating its individual intake based on food questionnaire, and didn't find any. And it is known that CLA does inhibit mammary carcinogenesis in in vitro experiments (laboratory experiments directly exposing sample cells to a chemical agent). The problem is not only that a questionnaire is unreliable source of information; it is also impossible to estimate CLA intake with anything resembling accuracy, due to the fact that its content in these foods varies widely depending on the animal feed (it is up to several times higher in animals fed on grass, than those fed with grains). Another hurdle is that body's ability to utilize these essential fatty acids (EFA), and particularly to synthesize longer-chain EFAs from short- and medium-chain EFAs like CLA, depends on one's enzymatic efficiency, which also varies widely individually. Yet another is that if the relative quantity of these fatty acids is small vs. non-essential fats, or other EFAs (much less likely) - about 1 in 20, or smaller - their utilization by the body is inhibited, and can even further deplete its body reserves (this is, for instance, the case with beef, whose low CLA content is effectively wasted due to the relatively high beef content of non-essential oleic fatty acid). None of these factors, or any others (there is certainly much more to it, since any effect, positive or negative, of one nutrient can be reinforced, or neutralized by a number of other individual factors) were mentioned in the study. It simply estimated the CLA "paper" intake based on food quantities entered into food questionnaire and published data on its food contents. And that's where study's yet another, hopeless shortcoming becomes glaringly obvious. The calculated CLA intake ranged from >78mg to >156mg a day, from the lowest to highest quintile, respectively. The official U.S. recommendation for linoleic acid is as much as 5-10% of the total calories, while Udo Erasmus estimates the optimum intake as 3-6%, with about 1/3 of it being necessary to prevent deficiency in most people. Taking 2% as the reasonable minimum preventing deficiency, and 2000 cal/day diet, gives 40 calories from linoleic acid which, at 9 calories per gram, comes to 4.4g. In other words, the highest intake quintal in the study was still only 4%, or so, of the minimum recommended intake! How much of a beneficial effect could have ingesting 4% instead of 2% of the safe minimum of any nutrient? Shouldn't they know better? The authors do mention, at the bottom of the paper, that the lack of association could be due to the CLA intake being below the level needed to provide protective effect (not specified), but that doesn't prevent them from concluding that: "The results provide no evidence of a protective effect of CLA against breast cancer development in women.". Such conclusion is "substantiated" as being an analysis of responses from 66,433 women in 1987-90 and 36,664 women in 1997 follow up. And it does get quoted in other studies and articles, as if it actually means something. This study may be among the more drastic examples, but literally all of them are flawed by neglecting the vary basic fact that breast cancer is a heterogeneous disease resulting from a multitude of internal and external factors, varying in number, individual importance and interactions from one women to another. Instead of trying to untie the knot by pulling which ever loose end seems to be sticking out, based on any criterion that happened to be the "priority", the only path to the solution is to slowly, methodically and patiently arrive to the answer by following all the ends to the core of the knot. And that means parting with the statistical, fly-by approach of looking for causal links with a few more or less randomly selected parameters in a study population that is not controlled for such a basic element as a complete nutritional status, let alone individual metabolism, toxic exposures and sensitivities. If we are to find what is causing disruption of the normal cell cycle, we have to look at all the relevant factors involved. Simple as that. And, yes, it cannot be accomplished without individualizing study approach. As it is, unfortunately, research "evidence" produced by most health-related studies in general, and breast cancer related ones in particular, is not just unreliable, they are also only statistically applicable. At best, it tells you what seem to matter for the majority of women - but does it, and how much apply to you, the individual? You can only guess, and so can your doctor. It is well known, in both medical research and practice, that one same food can be beneficial for one individual, while without effect or even harmful for the other. How does the statistical approach, focusing on the numbers for large groups of individuals, address, i.e. control this fact? It doesn't. Again, conclusions of "no association", "strong association", "suggestive evidence" or "no evidence" mean little coming from study populations whose vital
individual determinants of body function - It is inevitable that researchers, failing to correct for this chronic fundamental omission, remain in dark. Here's an example of that kind of "evidence", according to one of the recent studies on the subject:
1
may be restricted to hormone sensitive breast
cancers
2
possible The summary (Opportunities and Strategies for Breast Cancer Prevention Through Risk Reduction, Mahoney et al. 2008) is mainly based on the Nurses' Health Study trials, which are of observational type, depending on information obtained through food questionnaires. Subjectivity and uncertain reliability of the main source, and the fact that any given study was focused on a (very) limited set of factors which, in addition, often are not effectively controlled, makes the results useful only for rough guidance at best. For instance, when intake of polyunsaturated fats is among factors focused on by a study, it is nearly always for the total of polyunsaturated fats. There is a big difference between refined corn or sunflower oil on one side, and natural hemp or flax oil on the other. The former are unhealthy fats, the later are healthy, but they all go under the same dietary factor, "polyunsaturated fat intake". It also matters very much whether these fats are heated in use, and to what extent, or not, but that "detail" is simply left out. Or, if you are interested in how was folic acid identified as a probable factor at least partly offsetting the negative effect of alcohol consumption, the more important point from the study was largely ignored, which is that women obtaining folate from multivitamin/mineral supplements had 26% lower incidence of breast cancer, compared to 5% excess risk in those taking folate supplementation alone, and 32% excess risk in those with no nutritional supplementation (Zhang et al. 1999). Obviously, the numbers indicate that the protective effect comes mainly from taking multimineral/vitamin supplementation - which is in line with the known fact that alcohol consumption depletes nutrients - and not from folic acid alone. Way to design and interpret studies? Not if we are looking for meaningful conclusions. And, of course, treatment of polyunsaturated fat intake is just a drop in the ocean, but illustrative of why breast cancer research seems to be roaming in a circle. This is why the effect of dietary factors in these studies is far from being consistent, just as it has been with other types of studies included in the analysis. Of course, we don't really need studies to tell us that what we put
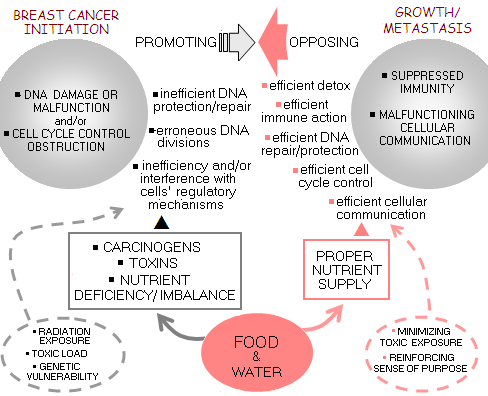
Only - if they can - in which particular ways. Preferably, with a customized, individualized approach. Statistical associations, regardless of how trendy they are in modern medicine, are not just inherently unreliable. They are plain inapplicable to any individual woman, or any specific breast cancer case. Sketch below illustrates the very basic dependence of breast cancer initiation and growth on the food factor. Simply put, the body needs optimum intake of nutrients in order to function optimally; any significant longer term deviation from such intake compromises its functions, making it more vulnerable to health disorders, including cancer. Dashed lines mark other major factors in (breast) cancer initiation and growth.
Unfortunately, there is no such thing as "standard optimized diet". Nor, for that matter, any form of food culture that one could depend on for making right dietary choices - at least in general. And it wouldn't be enough, if we'd have it. Because not all good foods are good for everyone, and some may even be harmful. Nutritional needs and tolerances vary from one individual to another, and for any given individual with time and health status. Luckily, there are general dietary guidelines with respect to healthy diet, which even the official medicine - long time ignoring or denying any significance of diet in the health matters - increasingly acknowledges. It is the best starting point, but optimized diet has to be individually tailored - something that requires individual's initiative and effort. The importance of finding such diet and adhering to it, again, varies individually. Those at increased risk of breast cancer have a very good reason to go for it. With this in mind, let's set some general remarks with respect to dietary factors generally significant in the context of breast cancer, and why. Let's start with the negatives. Dietary factors predisposing for and promoting breast cancer First, caloric intake. It is recognized that higher caloric intake tends to increase breast cancer risk. Looking at the world's population, there is a solid direct association between higher caloric intake and increased rates of breast cancer. What complicates the picture are many confounding factors, both known and unknown, varying in magnitude from one population to another. Still, caloric intake alone is a likely significant factor, and may be particularly important in childhood, modifying body metabolism to stimulate growth, i.e. hormonal activity. The two macronutrients mainly responsible for the caloric intake level are fat and sugar (practically referring to refined sugar, or sucrose). Both are associated with increased estrogen level. And, in addition to their caloric contribution, either can, and very likely does, negatively affect breast cancer risk in a number of ways. It is often cited that high-fat diet promotes breast cancer, but it is more than just fat issue. Such diets are typically unhealthy in many other aspects, such as significant intake of highly processed, denatured, chemically contaminated and nutritionally depleted foods, unhealthy refined fats and trans-fatty acids, high intake of saturated fats from animal-origin foods, low plant foods dietary fiber intake, low intake of good fats and essential fatty acids, low level of physical activity, higher average consumption of alcohol and/or refined sugars, and so on. It boils down to the body hampered by lowered nutritional intake and/or gross nutritional imbalances, while at the same time subjected to the higher toxic exposures. That, obviously, makes it more vulnerable. High intake of the animal-origin foods - particularly animal fats - is all but certain to result in high intake of toxic chemicals. Just like ours, animal bodies tend to store toxins they cannot eliminate in the fat tissue; considering that growing one pound of animal protein requires average consumption (by the animal) of 20 times as much of plant protein, indicates inevitably significantly higher
concentrations of environmental toxins in than in plant-origin foods. And, in addition to the toxins already present in their feed, animals grown for food are also exposed to chemicals added to it. Another danger of the excessive consumption of animal-origin foods is the absence of dietary fiber. In addition to other healthful effects of dietary fiber - particularly aiding in removal of toxins from the intestines - its insoluble portion also absorbs estrogenic hormones deactivated by the liver and excreted to the intestines via bile, inhibiting their re-absorption into the circulation. High-sugar diet is also typically low in nutrients, and generally unhealthy; that combines poorly with the fact that even moderate amounts of sugar, 50-100g, suppress activity of the immune system up to 50%, possibly even more, for hours after consumption. This means that those on high sugar intake have the immune function seriously suppressed good portion of the time. Sugar also stimulates production of the inflammatory prostaglandin E2, that can promote cancerous growth. Furthermore, sugar elevates glucose level, which in turn stimulates secretion of insulin - a hormone that by stimulating cellular proliferation, can fuel breast cancer similarly to estrogen. Low-oxygen, high-glucose environment is ideal for the metabolism of cancerous cell; hence high-sugar diet (i.e. high glycemic index diet) combined with shallow breathing and physical inactivity creates generally favorable environment for cancerous growth. At the cellular level, one of the chief waste products of glucose metabolism, lactic acid, increases acidity, which has many negative consequences on the cellular homeostasis, including impaired use of oxygen. At the extreme end of this overall high-sugar-diet-induced trend is the cancer cell, regressed to its primitive form of metabolism, living on burning glucose in an oxygen-deprived, acidic environment (glycolysis). Body regulation of the level of another hormonal substance, similar to insulin in its stimulatory effect on cell proliferation, insulin-like growth factor (IGF), is also directly affected by dietary patterns. While study results are inconsistent in establishing the relationship between a number of diet-related factors and IGF levels, evidence suggests that IGF levels generally move inversely to the caloric and protein intake. The fact that the two principal IGF forms, IGF-I and IGF-II are controlled by at least seven different IGF binding proteins, some of which suppressing, and the others enhancing their activity, illustrates part of the reasons behind the difficulty to consistently relate IGF body levels to their effect on breast cancer. Combined with other known and unknown factors influencing IGF activity, or breast cancer risk in general, as well as with the limitations of study designs and techniques, it is bound to make study results unpredictable. As already mentioned, this uncertainty is rather common, to a greater or lesser degree, to nearly all breast cancer factors. There is just to many disease variables on one, and limited knowledge, tools and resources on the other side, to allow arriving at consistent, reliable statistical results. And, as already pointed out, even if we'd have reliable statistical results, their usefulness in any specific case would be also only of statistical value, at the best. These were the main negative dietary factors, making the body more vulnerable to breast cancer. What kind of a diet is protective against it? Dietary factors strengthening the body against breast cancer As we said already, such diet has to be individually optimized. But some general rules still apply. We could start with a diet that lowers estrogen levels. It should be: ● plant, or predominantly plant-based ● no added sugar ● (good) fats limited to less than 30% of calories Simple as that. Why plants? Because high-fiber foods and an overall healthier gut enhance elimination of estrogen: women vegetarians have 2 to 3 times higher rate of estrogen elimination, and 50% lower free estrogen blood level than omnivores. Because plant phytoestrogens - particularly those in soy foods, but also others, for instance in licorice - exert estrogen-protective effect by clinging to the cellular estrogen receptors while having less than 2% of estrogen's potency. This effectively lowers estrogen activity. And because both, high-sugar and fat diets commonly lead to the formation of significant body fat tissues, which produce estrogen of their own. The additional hallmark of such diet is nutrient deficiency, and/or imbalance, which further worsen body's ability to control estrogen levels. Guy Abraham's PMS (premenopausal syndrome) population sample was found to be consuming 62% more refined carbs, 275% more refined sugar, 79% more dairy and 78% more sodium than symptom-free population sample - which is safe to assume as already having undesirably high intakes of these food items. And PMS is commonly caused by - you know it - elevated estrogen levels. Not the least it is due to the compromised liver function (cholestasis) due to nutritional deficiencies - particularly vitamin B6, or nutrients needed for the conversion into its active form - bad intestinal bacteria, lack of dietary fiber, and other common consequences of this type of diet, all of which present obstacle to the efficient removal of estrogen from the bloodstream. Of course, there is much more to the breast cancer protective diet than just helping control body's estrogen metabolism. But the basic recipe is just as simple: maximize nutrients - minimize toxins And plant-based diet happened to best fit this requirement. Not just any plant-based diet, but the whole-food plant based diet. Because plants do get processed and turned into low-nutrient high-toxins (chemical additives, unhealthy fats, excess sugar, etc.) foods as well. Just eliminating processed foods would make the typical American diet much healthier, hence also more protective against breast cancer and other diseases. What you eat matters more than any other single controllable factor that can predispose you for breast cancer. But the rest of them, especially combined, shouldn't be neglected. More about those other predisposing breast cancer factors on next page. YOUR BODY ┆ HEALTH RECIPE ┆ NUTRITION ┆ TOXINS ┆ SYMPTOMS |
||||||||||||||||||